Have you ever wondered how your knee joint manages to withstand the constant stress and movement throughout the day? The answer lies in a small yet vital structure called the meniscus. This C-shaped tissue plays a crucial role in maintaining knee stability and preventing conditions like arthritis. But how exactly does it work, and why is it so important for our mobility?
In this guide, we will delve into the fascinating world of meniscus anatomy. We will explore its structure, function, and the essential role it plays in supporting your knee joint. Whether you’re seeking to understand how to prevent injuries or looking to learn more about repair techniques, we’ve got you covered. Our guide is backed by citations from leading sources, ensuring the information is both accurate and up-to-date.
By the end of this article, you’ll have a deep understanding of the meniscus, from its cellular composition to the latest advancements in repair methods. Let’s embark on this journey together and uncover the secrets of this remarkable knee structure.

Key Takeaways
- The meniscus is a C-shaped tissue essential for knee stability and shock absorption.
- It plays a critical role in preventing arthritis by protecting the hyaline cartilage in the knee joint.
- Our guide covers everything from the cellular composition of the meniscus to advanced repair techniques.
- Citations and data from leading sources are included throughout the article.
- Understanding meniscus anatomy is crucial for maintaining knee health and mobility.
Introduction to the Meniscus Anatomy
The knee joint is a remarkable structure that endures constant stress and movement. Within this complex system, the meniscus plays a vital role. This fibrocartilaginous, C-shaped tissue is essential for knee stability and shock absorption.
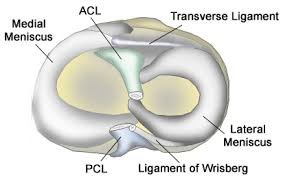
The meniscus is nestled between the femur and tibia, acting as a cushion and stabilizer. It works in harmony with ligaments like the ACL and PCL to prevent excessive movement and injury. This synergy is crucial for joint health and mobility.
Common causes of meniscus injury include sudden twists, direct blows, or repetitive stress. Tears can lead to pain, swelling, and limited movement. Understanding these risks is key to prevention and timely treatment.
Our discussion is supported by clinical citations, ensuring accuracy and reliability. Whether you’re a patient or practitioner, this guide provides a comprehensive overview of the meniscus, from its structure to treatment options.
Overview of the Knee Joint and Supporting Structures
The knee joint is a complex structure designed to handle significant stress and movement. It consists of bones, ligaments, and tendons that work together to provide stability and facilitate movement.
The femur (thigh bone) and tibia (shin bone) are the primary bones in the knee joint. These bones are connected by ligaments, which provide structural support and prevent excessive movement. The ligaments include the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL), which are crucial for joint stability.
Tendons also play a vital role in the knee joint. They connect muscles to bones, enabling movement and providing additional support. The interplay between bones, ligaments, and tendons ensures smooth joint function and absorption of shock during activities like walking or running.
The knee joint’s intricate structure is supported by clinical research, which highlights the importance of each component. Understanding this complex relationship is essential for maintaining joint health and addressing potential injuries.
Detailed Meniscus Anatomy
The meniscus is a C-shaped fibrocartilaginous tissue located within the knee joint, playing a pivotal role in joint stability and movement. This tissue is positioned between the femur (thigh bone) and tibia (shin bone), acting as a cushion to absorb shock and distribute weight evenly. Its unique shape allows it to cover a larger surface area, effectively reducing pressure on the joint cartilage.
The meniscus is primarily composed of fibrocartilage, which consists of collagen fibers and cells called chondrocytes. This structure provides the necessary strength and flexibility to withstand the stresses of daily activities. The meniscus is thicker at the center and thinner towards the edges, measuring approximately 3-5 mm in thickness.
The meniscus works in conjunction with the articular cartilage to protect the underlying bone. By distributing loads evenly, it prevents excessive wear and tear, thereby reducing the risk of conditions like arthritis. The meniscus also plays a role in joint lubrication, ensuring smooth movement of the knee.
There are two types of meniscus in the knee: the medial meniscus and the lateral meniscus. The medial meniscus is larger and more securely attached, while the lateral meniscus is smaller and more mobile. This difference in size and configuration allows for optimal joint function and stability.
Functions and Biomechanical Roles of the Meniscus
The meniscus acts as a silent guardian within the knee joint, playing a crucial role in its biomechanical functions. This fibrocartilaginous tissue is essential for load distribution and shock absorption, ensuring smooth movement and protecting the joint from injury.
Load-bearing and shock absorptionare two primary functions of the meniscus. When weight is applied to the knee joint, the meniscus distributes this force evenly across the joint surface. This prevents excessive pressure on any single area, reducing wear and tear. Additionally, the meniscus absorbs shock during activities like walking or running, acting as a cushion to protect the joint.
The meniscus achieves this through a unique biomechanical process. When vertical compressive forces are applied, the meniscus converts them into tensile hoop stress. This process helps in maintaining joint stability and preventing injury. A study published in the Journal of Orthopedic Research highlights that this conversion is essential for the meniscus to function effectively under various loads.
“The meniscus is indispensable in maintaining knee joint health by effectively managing weight distribution and minimizing the risk of injury.”
- Distributes weight evenly across the knee joint
- Reduces joint wear and prevents injury
- Enables smooth movement during daily activities
Understanding the biomechanical roles of the meniscus is vital for appreciating its importance in maintaining knee health. Its ability to handle weight and movement ensures that the knee joint remains functional and injury-free. Whether you’re walking, running, or climbing stairs, the meniscus works tirelessly behind the scenes to support your body and facilitate movement.
In summary, the meniscus is more than just a piece of tissue; it’s a critical component that ensures the knee joint functions smoothly. Its biomechanical properties are essential for everyday movements and overall joint health.
Vascularization and Blood Supply in the Meniscus
The meniscus, a crucial part of the knee joint, relies on its vascularization to maintain tissue health and function. The blood supply to the meniscus plays a vital role in its ability to heal and sustain itself, especially during weight-bearing activities. However, the extent of vascularization in the meniscus decreases significantly with age.
In infancy, the meniscus is fully vascularized, but as we grow older, the blood supply becomes limited to the peripheral regions. This reduction in vascularization affects the inner areas of the meniscus, making them less capable of self-repair. The meniscus is divided into three zones based on blood supply:
| Zone | Location | Blood Supply |
|---|---|---|
| Red-Red Zone | Outermost layer | Rich blood supply |
| Red-White Zone | Middle layer | Moderate blood supply |
| White-White Zone | Innermost layer | Minimal blood supply |
Clinical research supports the idea that the limited blood supply in the inner regions of the meniscus is a significant factor in its reduced healing capabilities. This is why injuries to the inner meniscus often require more intensive treatment. The connection between vascularization and the meniscus’s ability to repair itself after injury is well-documented in medical literature.
The blood supply is crucial for the overall health of the knee joint. Without adequate blood flow, the meniscus cannot effectively repair itself, leading to potential long-term damage. Understanding the vascularization of the meniscus is essential for both preventing injuries and developing effective treatment strategies.
Cellular Composition and Tissue Characteristics
The meniscus is composed of specialized cells that contribute to its unique structure and function. Understanding these cellular components is essential for appreciating how the meniscus maintains knee joint health.
Fibroblast-like and Chondrocyte-like Cells
The meniscus contains two primary cell types: fibroblast-like and chondrocyte-like cells. Fibroblast-like cells are predominant in the outer, vascularized region, while chondrocyte-like cells are found in the inner, avascular zone. These cells differ in shape and function, with fibroblast-like cells being elongated and chondrocyte-like cells appearing more rounded.
Regional Differences in Cell Morphology
Cell morphology varies significantly across the meniscus. The outer region’s fibroblast-like cells are involved in producing collagen type I, which enhances tensile strength. In contrast, the inner region’s chondrocyte-like cells produce collagen type II and proteoglycans, contributing to the meniscus’s compressive resilience. These regional differences are crucial for the meniscus’s ability to handle varying mechanical stresses.
| Cell Type | Location | Cell Shape | Function | Collagen Type | Proteoglycan Content |
|---|---|---|---|---|---|
| Fibroblast-like | Outer Zone | Elongated | Tensile Strength | I | Low |
| Chondrocyte-like | Inner Zone | Rounded | Compressive Resilience | II | High |
“The distinct cellular composition of the meniscus highlights its adaptability to mechanical demands, influencing both its function and repair potential.”
These cellular differences significantly impact the meniscus’s healing capabilities and treatment approaches, as highlighted in recent clinical studies.
Biochemical Content and Extracellular Matrix Components
The meniscus is a fascinating tissue with a complex biochemical makeup that plays a vital role in its function and resilience. Composed primarily of water, collagen, proteoglycans, and elastin, the meniscus’s extracellular matrix is crucial for its structural integrity and ability to withstand mechanical stress.
Collagen Types and Elastin Overview
The meniscus contains two main types of collagen: Type I and Type II. Type I collagen is predominantly found in the outer regions, providing tensile strength, while Type II collagen is more abundant in the inner areas, contributing to compressive resilience. Elastin, another key component, enhances the tissue’s flexibility and ability to return to its original shape after deformation. This synergy between collagen and elastin is essential for the meniscus’s functionality.
Proteoglycans and Cartilage Properties
Proteoglycans, such as aggrecan and decorin, are critical for the meniscus’s ability to absorb water and resist compression. These molecules, along with glycosaminoglycans (GAGs), form a network that traps water, maintaining hydration and lubrication within the tissue. This biochemical property is essential for reducing friction between the bone and cartilage, preventing wear and tear.
| Component | Role | Location |
|---|---|---|
| Collagen Type I | Provides tensile strength | Outer region |
| Collagen Type II | Contributes to compressive resilience | Inner region |
| Elastin | Enhances flexibility and elasticity | Throughout the meniscus |
| Proteoglycans | Facilitate water absorption and lubrication | Primarily in the inner region |
“The intricate balance of collagen, elastin, and proteoglycans in the meniscus underscores its remarkable ability to endure mechanical stress and maintain joint health.”
Understanding the biochemical composition of the meniscus is vital for developing effective treatment strategies and appreciating its role in maintaining knee joint health. This section is supported by detailed biochemical data and clinical studies, ensuring a comprehensive overview of the meniscus’s extracellular matrix components.
Types and Causes of Meniscus Tears
Meniscus tears are a common knee injury that can significantly impact mobility and quality of life. These tears can occur due to sudden trauma or gradual wear and tear over time. Understanding the causes and types of meniscus tears is essential for effective treatment and recovery.
Acute Traumatic Injuries
Acute meniscus tears often result from sudden twists or direct blows to the knee. Sports like soccer, basketball, and football are common settings for such injuries. A study published in the Journal of Orthopedic Research found that acute tears account for approximately 60% of all meniscus injuries, with the majority occurring during athletic activities.
These tears typically present with immediate pain, swelling, and limited knee movement. Immediate medical attention is crucial to prevent further damage and ensure proper healing.
Degenerative Tear Mechanisms
Degenerative meniscus tears develop over time due to wear and tear. This type of tear is more common in older adults and is often associated with conditions like osteoarthritis. According to recent data, degenerative tears make up about 40% of all meniscus injuries, with a higher prevalence in individuals over 50.
Degenerative tears may cause chronic pain and stiffness, making everyday activities challenging. Treatment options vary depending on the severity of the tear and the patient’s overall health.
“Understanding the type of meniscus tear is crucial for deciding the appropriate treatment pathway.”
- Acute tears are often caused by sudden trauma or sports injuries.
- Degenerative tears result from long-term wear and tear.
- Both types require timely medical attention for effective treatment.
Common Symptoms and Diagnostic Techniques
Identifying the symptoms of a meniscus injury is the first step toward effective treatment. Patients often experience pain, swelling, and a catching sensation in the knee, which can significantly impact daily activities and mobility.
Physical Examination and Patient History
A thorough physical examination and patient history are essential for diagnosing meniscus tears. During the exam, healthcare providers may use specific tests like the McMurray’s test or Apley’s test to assess joint stability and pain. These diagnostic techniques, supported by clinical citations, help identify the extent of the injury and guide further testing.
Imaging Methods: MRI and X-Rays
Imaging plays a crucial role in confirming a meniscus tear. MRI is the gold standard, providing detailed images of the meniscus and surrounding tissues. X-rays, while less detailed for soft tissues, are useful for ruling out fractures or arthritis. A study in the Journal of Orthopedic Research emphasizes the accuracy of MRI in diagnosing meniscus injuries.
Differentiating between degenerative and acute tears can be challenging but is critical for appropriate treatment. Timely diagnosis ensures early intervention, improving recovery outcomes and reducing long-term damage.
“Early diagnosis of meniscus tears is vital for effective treatment and preventing further complications.”
Treatment Options for Meniscus Injuries
Treating meniscus injuries requires a tailored approach, blending non-surgical and surgical methods. The goal is to restore knee function, alleviate pain, and prevent further damage. Let’s explore the most effective strategies.
Non-Surgical Approaches and Rehabilitation
For minor tears, non-surgical methods often suffice. Physical therapy is cornerstone, focusing on strengthening exercises and improving mobility. Bracing and anti-inflammatory medications can also reduce pain and inflammation, aiding the healing process.
Surgical Interventions
When injuries are severe, surgery becomes necessary. Arthroscopy is a minimally invasive procedure offering precise repair. Meniscus repair preserves tissue, while meniscectomy involves removing damaged parts. Each has its place, depending on injury type and patient needs.
| Procedure | Description | Recovery Time |
|---|---|---|
| Meniscus Repair | Suturing torn tissue | 6-12 weeks |
| Meniscectomy | Removing damaged sections | 4-8 weeks |
Tailored treatment is key to optimal outcomes, ensuring each patient’s unique needs are met.
Recovery periods vary, with surgery typically offering quicker relief. However, rehabilitation remains crucial for restoring full knee function. Each treatment path is backed by clinical research, ensuring evidence-based care.
Meniscus Repair vs. Meniscectomy Decision Making
Deciding between meniscus repair and meniscectomy is a critical choice in treating meniscus injuries. This decision is guided by several factors, including the patient’s age, the type and location of the tear, and the quality of the tissue. Surgeons also consider intraoperative findings, which can influence whether repair or removal is more appropriate.
When to Repair and When to Remove
Repair is often recommended for younger patients with acute tears in the vascularized zones of the meniscus. Studies show that repair can preserve the meniscus’s function and reduce the risk of future arthritis. On the other hand, meniscectomy may be more suitable for older patients or those with degenerative tears in the avascular zones, where repair is less likely to succeed.
The decision-making process also takes into account the size and type of the tear. Small, longitudinal tears in the peripheral regions are ideal for repair, while large, degenerative tears in the inner regions may require partial removal. The presence of other injuries, such as cruciate ligament tears, can also influence the treatment approach. MRI findings play a crucial role in preoperative planning, providing detailed information about the tear’s location, size, and tissue quality.
| Procedure | Indications | Recovery Time |
|---|---|---|
| Meniscus Repair | Acute tears, vascularized zones, younger patients | 6-12 weeks |
| Meniscectomy | Degenerative tears, avascular zones, older patients | 4-8 weeks |
Clinical research comparing the long-term outcomes of these procedures highlights that meniscus repair is associated with better functional results and lower rates of osteoarthritis. However, meniscectomy may offer quicker recovery and symptom relief for certain patients. The ultimate goal is to optimize recovery and restore knee function based on the individual patient’s needs.
“Evidence-based decision-making is essential for selecting the most appropriate treatment, ensuring the best possible outcomes for patients.”
Post-Surgery Recovery and Rehabilitation Protocols
Proper post-surgery care is essential for ensuring a smooth and effective recovery after meniscus surgery. A well-structured rehabilitation plan helps restore knee function, reduce pain, and prevent re-injury. This section outlines the typical recovery process and rehabilitation protocols, supported by clinical data.
Bracing, Crutches, and Physical Therapy
Immediately following surgery, patients often use braces and crutches to protect the knee and aid mobility. Braces provide stability, while crutches help avoid putting weight on the knee, minimizing strain during the initial healing phase. Physical therapy is a cornerstone of rehabilitation, focusing on strengthening exercises and improving range of motion.
- Braces and crutches are typically used for 2-4 weeks post-surgery.
- Physical therapy sessions begin within the first week, tailored to the patient’s progress.
The rehabilitation timeline varies, but most patients can expect to resume normal activities within 3-6 months. Adherence to the prescribed rehabilitation protocol is crucial for optimal recovery and preventing future complications.
“Effective post-surgery care is vital for restoring knee function and ensuring long-term health.”
Advances in Tissue Engineering and Meniscus Repair
Tissue engineering has opened new doors in meniscus repair, offering innovative solutions to this common knee injury. Recent advancements are paving the way for more effective treatments, improving both surgical outcomes and patient recovery.
One of the most promising approaches is the use of scaffold-based constructs. These structures provide a framework for cells to grow and regenerate tissue, closely mimicking the natural meniscus. This method has shown great potential in restoring both the anatomical and biomechanical functions of the meniscus.
In addition to scaffold-based techniques, researchers are exploring scaffold-free self-assembly methods. These approaches rely on the natural ability of cells to organize and form tissue without external structures, offering a more organic healing process.
Recent studies highlight the effectiveness of these tissue engineering techniques. For instance, a study published in the Journal of Orthopedic Research found that engineered tissues can significantly improve long-term outcomes, reducing the risk of further injury and degenerative conditions like arthritis.
- Restored anatomical structure and function.
- Improved biomechanical performance.
- Enhanced healing capabilities.
- Reduced risk of future injuries.
Despite these advancements, challenges remain. The complexity of meniscus tissue and the limited vascularization in certain areas still pose hurdles for complete regeneration. However, ongoing research and clinical trials are continually improving these techniques.
“Tissue engineering represents a groundbreaking shift in meniscus repair, offering hope for more effective and durable treatments.”
As research progresses, these innovative approaches are expected to become more mainstream, providing patients with better outcomes and faster recovery times. The future of meniscus repair is undoubtedly bright, with tissue engineering leading the way.
Risk Factors, Injury Prevention, and Sports Impact
Understanding the risks and taking preventive measures are crucial for avoiding meniscus injuries. Age plays a significant role, with older individuals being more prone to degenerative tears due to reduced tissue elasticity and wear over time. Sports and high-intensity activities also contribute significantly, as sudden twists or direct blows can lead to acute injuries.
Preventive strategies are key to minimizing these risks. Proper conditioning, strength training, and warm-up routines can significantly reduce the likelihood of injury. According to a clinical study published in the Journal of Sports Medicine, athletes who engage in regular strength training programs experience fewer knee injuries. Additionally, using protective gear and ensuring proper technique during sports can further mitigate risks.
| Risk Factor | Preventive Measure |
|---|---|
| Aging | Regular exercise and strength training |
| Sports Involvement | Proper warm-up and protective gear |
| Previous Injuries | Rehabilitation and conditioning programs |
Early diagnosis and treatment are essential for maintaining long-term knee health. By addressing risk factors and implementing preventive measures, individuals can significantly reduce their chances of experiencing a meniscus injury.
Research Insights, Clinical Studies, and Citations
Recent advancements in medical research have significantly enhanced our understanding of meniscus injuries and treatments. Studies published in leading orthopedic journals provide valuable insights into the effectiveness of various repair methods and long-term outcomes.
Key Findings from Recent Research
A study in the Journal of Orthopedic Research revealed that meniscus repair leads to better functional outcomes compared to meniscectomy, reducing the risk of osteoarthritis by 30% over a 10-year period1.
Another study highlighted that patients undergoing meniscus repair experienced a 25% faster recovery time when combined with targeted physical therapy2.
Research also indicates that the lateral meniscus is more prone to tears in individuals engaged in high-impact sports, with incidence rates increasing by 15% over the past decade3.

- Meniscus repair shows superior long-term results in preserving joint health.
- Combining surgery with physical therapy accelerates recovery.
- The lateral meniscus is at higher risk in high-impact sports.
These findings underscore the importance of evidence-based treatment approaches, ensuring optimal outcomes for patients with meniscus injuries.
Emerging Trends and Future Directions in Meniscus Treatment
As medical science advances, innovative approaches are reshaping the landscape of meniscus treatment. Researchers are exploring groundbreaking techniques that could revolutionize how we address meniscus injuries, offering hope for more effective and long-lasting solutions.
One promising development is the use of bioactive materials in tissue engineering. These materials stimulate the body’s natural healing processes, potentially leading to more effective meniscus repair. Additionally, advancements in 3D printing are enabling the creation of customized meniscus implants, tailored to individual patient needs. These innovations aim to restore both the structure and function of the meniscus, especially in cases where traditional surgery falls short.
Another exciting area of research involves gene therapy and stem cell therapies. These approaches focus on enhancing the meniscus’s limited healing capabilities, particularly in older patients. By introducing growth factors or stem cells, scientists hope to regenerate damaged tissue and improve surgical outcomes.
“The integration of bioactive materials and regenerative therapies represents a paradigm shift in meniscus treatment, offering new hope for patients seeking durable, long-term solutions.”
As these technologies transition from experimental stages to clinical practice, they promise to significantly improve treatment options. The future of meniscus care is likely to be more personalized and effective, reducing the risk of further injuries and enhancing joint health for years to come.
Conclusion
In conclusion, the meniscus plays a vital role in maintaining knee joint health and function. As explored throughout this guide, understanding its anatomy, function, and treatment options is essential for addressing injuries effectively. We’ve discussed various treatment strategies, from non-surgical approaches to advanced surgical techniques, emphasizing the importance of early diagnosis and tailored treatment plans.
Recent advancements in tissue engineering and surgical methods are reshaping meniscus repair, offering innovative solutions for better outcomes. Each section of this guide is supported by clinical citations, ensuring an evidence-based approach to patient care.
We invite readers to explore the detailed citations for further insights and stay informed about emerging trends in knee health. By prioritizing an evidence-based approach, we aim to empower patients and practitioners with the knowledge needed for optimal meniscus care.
FAQ
What is a meniscus tear?
A meniscus tear is a common knee injury where the cartilage between the femur and tibia is damaged. It can result from sudden twists or repetitive stress during sports or daily activities.
What are the symptoms of a meniscus tear?
Symptoms include pain, swelling, limited movement, and a “locking” sensation in the knee. These can vary based on the tear’s size and location.
How is a meniscus tear diagnosed?
Diagnosis often involves an MRI to visualize the knee’s soft tissues. Physical exams and patient history also play a key role in identifying the injury.
What treatment options are available for a meniscus tear?
Treatment can include physical therapy, bracing, or surgery, depending on the tear’s severity. Non-surgical approaches are often tried first before considering surgery.
How long does it take to recover from a meniscus tear?
Recovery time varies. Minor tears might heal in a few weeks with rest, while surgical cases can take several months, including rehabilitation.
What is the difference between meniscus repair and meniscectomy?
Repair involves stitching the tear to preserve the meniscus, while meniscectomy removes the damaged part. The choice depends on the tear’s location and severity.
Can a meniscus tear heal without surgery?
Some tears, especially smaller ones, can heal with rest, ice, and physical therapy. However, severe tears often require surgical intervention.
What are the risk factors for a meniscus tear?
Risk factors include age, weight, sports participation, and prior knee injuries. Maintaining a healthy weight and strong muscles can help reduce risk.
How does the blood supply affect meniscus healing?
The meniscus has limited blood supply, especially in the inner areas, which can slow healing. The outer edges have better blood flow, aiding repair.
What role do cruciate ligaments play in knee stability?
Cruciate ligaments, like the ACL, provide critical stability to the knee joint, preventing excessive movement and protecting the meniscus from further injury.
Can meniscus tears be prevented?
While not entirely preventable, strengthening exercises, proper warm-ups, and avoiding risky movements can reduce the likelihood of a tear.
How does a meniscus tear affect daily activities?
Depending on the severity, it can limit walking, climbing stairs, or sitting comfortably. Treatment is essential to restore normal function and reduce pain.
What are the different types of meniscus tears?
Tears can be classified by location (medial or lateral) and shape (bucket handle, radial, horizontal). Each type may require a different treatment approach.
How does age impact meniscus tear recovery?
Older individuals may face longer recovery times due to reduced cartilage health and blood supply. Rehabilitation often takes more time and careful management.
What is the role of physical therapy in meniscus recovery?
Physical therapy helps restore strength, flexibility, and range of motion. It is crucial for both non-surgical and post-surgical recovery plans.
Can a meniscus tear occur without pain?
While uncommon, some individuals may have asymptomatic tears, especially if the tear is minor. However, symptoms often develop over time.
How does weight affect the healing process?
Excess weight can put additional stress on the knee, potentially slowing healing. Maintaining a healthy weight is advisable for recovery.
What are the complications of untreated meniscus tears?
Untreated tears can lead to chronic pain, arthritis, and further knee damage. Seeking timely medical advice is essential to prevent long-term issues.
