Have you ever wondered why bending your legs can trigger sharp discomfort—even without visible inflammation? This puzzling sensation affects millions, yet many dismiss it as temporary strain. Let’s uncover why your joint might protest during simple movements like climbing stairs or sitting.
Our joints endure daily stress, but their intricate design also makes them prone to hidden issues. Tendons, ligaments, and cartilage work together seamlessly—until something disrupts their harmony. Overuse, aging, or subtle injuries often explain this type of ache, but pinpointing the source requires deeper insight.
We’ll guide you through the most frequent culprits behind these symptoms. From runner’s knee to arthritis precursors, identifying patterns in your discomfort is the first step toward relief. Remember: persistent soreness deserves attention, even if swelling isn’t present.
Key Takeaways
- Discomfort during bending often stems from overuse, alignment issues, or early-stage conditions.
- Daily activities like exercising or sitting for long periods can strain joint tissues.
- Cartilage wear or tendon irritation frequently causes pain without visible inflammation.
- Professional evaluation is crucial for chronic or worsening symptoms.
- Understanding your joint’s anatomy helps recognize warning signs early.
Understanding Knee Anatomy and Function
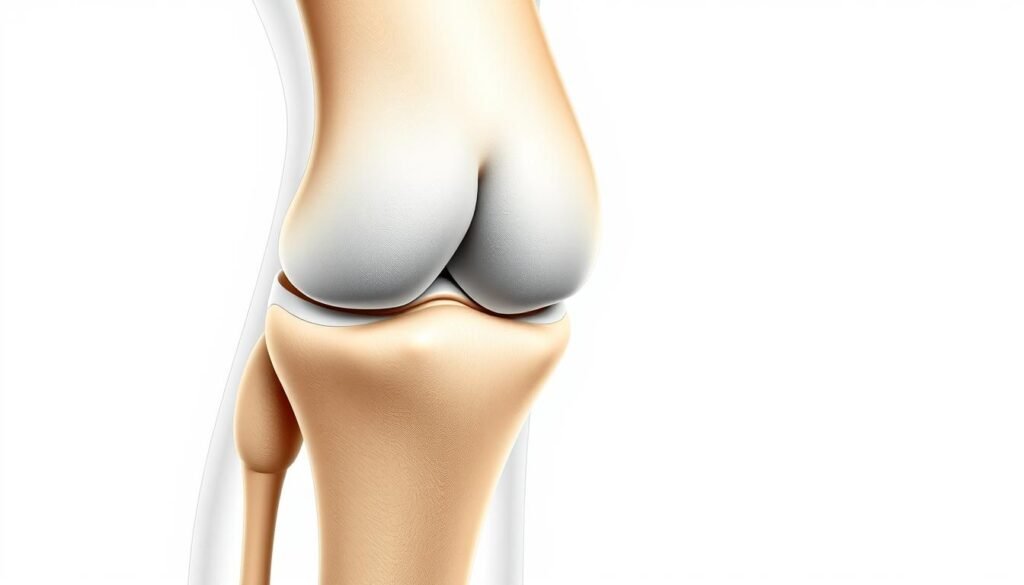
The human body’s largest joint plays a critical role in everyday mobility. Four bones—the femur, tibia, patella, and fibula—form its foundation. These structures work with soft tissues to handle forces up to five times body weight during movement.
Bones and Ligaments Overview
Thigh and shin bones connect through ligaments, which act like sturdy ropes. The anterior cruciate ligament (ACL) prevents forward sliding of the tibia. Medial and collateral ligaments add side-to-side stability, while the posterior cruciate ligament controls backward motion.
| Component | Function | Key Structures |
|---|---|---|
| Bones | Structural support | Femur, Tibia, Patella |
| Ligaments | Joint stability | ACL, PCL, MCL |
| Tendons | Muscle-bone connection | Quadriceps, Patellar |
| Cartilage/Bursae | Impact absorption | Meniscus, Synovial fluid |
Role of Tendons and Cartilage
Tendons anchor muscles to bones, translating contractions into motion. The patellar tendon, for example, powers leg extensions. Between bones, cartilage cushions impacts—the meniscus distributes weight, while articular cartilage allows smooth gliding.
Bursae—fluid-filled sacs—reduce friction during repetitive motions. When these components function harmoniously, the knee joint bends, twists, and bears weight effortlessly. Disruptions to this system often manifest as discomfort during specific activities.
Exploring Knee Pain Symptoms and Their Significance
Where your body sends distress signals matters more than you think. Discomfort patterns often reveal hidden problems long before visible signs appear. Let’s decode what different zones might indicate.
Identifying Pain Locations
Aching at the front of the joint often points to patellar tendon strain. Runners and cyclists frequently experience this during repetitive motions. Sharp twinges on the inner side could suggest medial meniscus wear.
Discomfort radiating from the back area demands special attention. One study notes:
“Posterior joint issues account for 15% of chronic mobility complaints, often overlooked during initial exams.”
| Location | Possible Condition | Common Triggers |
|---|---|---|
| Behind | Baker’s cyst | Prolonged sitting |
| Inner side | Medial arthritis | Twisting movements |
| Front | Patellofemoral syndrome | Stair climbing |
| Outer edge | IT band friction | Long-distance running |
Sudden stabs during squatting might signal cartilage damage. Dull throbbing after inactivity? Early-stage degenerative conditions sometimes start this way. Tracking symptom duration helps distinguish acute injuries from chronic issues.
Persistent soreness behind the joint could mean hamstring tendonitis or fluid buildup. Don’t ignore clicking sounds paired with instability—these symptoms often precede more serious complications. Early intervention prevents minor irritations from becoming major setbacks.
Knee Pain When Bending (No Swelling): Possible Causes
Understanding why movement triggers discomfort requires examining both sudden damage and gradual wear. While swelling often grabs attention, many issues create friction long before visible signs emerge. Let’s explore the hidden sources of strain that disrupt smooth joint function.
Common Medical Conditions
Patellofemoral syndrome often develops from repetitive stress. Runners and cyclists may notice a dull ache around the kneecap. Tenderness increases after prolonged sitting or stair use.
Tendonitis creates sharp twinges during bending motions. Ligament injuries frequently occur during sports that involve pivoting. A sudden twist can strain or tear connective tissues.
Injury Versus Overuse
Acute trauma—like a misstep or collision—often causes immediate sharpness. Overuse conditions, however, build gradually. Repetitive kneeling or jumping strains tissues over weeks.
| Cause Type | Key Features | Typical Triggers |
|---|---|---|
| Sudden Injury | Sharp pain during specific movements | Sports collisions, awkward landings |
| Overuse | Dull ache after repetitive actions | Running, prolonged kneeling |
Minor cartilage tears might not swell but still hinder mobility. Degenerative changes often start silently, revealing themselves through stiffness. Accurate identification of the root issue guides effective treatment plans.
Injury-Related Causes of Knee Pain
Physical activities often test our body’s resilience, especially in high-stress areas like the lower limbs. Sudden twists or impacts can disrupt critical structures that maintain stability. Let’s examine how specific injuries create persistent issues during movement.

Ligament Disruptions and ACL Complications
The anterior cruciate ligament (ACL) acts as a central stabilizer during pivoting motions. Athletes changing direction rapidly—like basketball players—often experience partial or complete tears. A study highlights:
“ACL injuries account for 40% of sports-related joint trauma, frequently requiring surgical intervention.”
Damage to the posterior cruciate ligament (PCL) typically occurs during car accidents or direct impacts. Unlike ACL tears, these injuries might not cause immediate instability but gradually weaken support structures.
Meniscus and Tendon Damage
Cartilage tears often produce sharp sensations when squatting or kneeling. The meniscus, which absorbs shock, can split during forceful rotations. Similarly, patellar tendon strains manifest as tenderness below the kneecap—common in volleyball players and sprinters.
| Injury Type | Common Signs | Recovery Timeline |
|---|---|---|
| ACL Tear | Audible pop, instability | 6–12 months |
| Meniscus Tear | Catching sensation | 3–6 weeks (minor) |
| Tendon Strain | Localized soreness | 2–8 weeks |
Ignoring these issues often worsens tissue damage. Orthopedic assessments using MRI or physical tests determine whether rest, therapy, or surgery offers the best path forward. Early diagnosis prevents long-term mobility limitations.
Degenerative and Inflammatory Conditions
Joint health can deteriorate silently, often revealing itself through persistent stiffness or grinding sensations. Unlike sudden injuries, these issues develop gradually—sometimes over decades. Early recognition of subtle changes helps prevent irreversible damage.
Osteoarthritis Versus Rheumatoid Arthritis
Osteoarthritis wears down cartilage between bones, creating bone-on-bone friction. This “wear-and-tear” condition often affects one side of the body first. Rheumatoid arthritis, an autoimmune disorder, attacks joint linings symmetrically. Both cause discomfort during bending but through different mechanisms.
“Early intervention in arthritis cases can reduce functional decline by 50%, according to recent rheumatology studies.”
| Condition | Primary Cause | Key Symptom | Treatment Approach |
|---|---|---|---|
| Osteoarthritis | Cartilage breakdown | Morning stiffness | Weight management, NSAIDs |
| Rheumatoid Arthritis | Immune system malfunction | Symmetrical joint issues | DMARDs, biologics |
Inflammation from these conditions irritates nerve endings, causing severe pain during movement. Degeneration reduces shock absorption, making stairs or crouching challenging. Those experiencing daily discomfort for over six weeks should consult a doctor.
Treatment strategies evolve with disease progression. Early stages may respond to over-the-counter anti-inflammatories and physical therapy. Advanced cases might require corticosteroid injections or joint replacement surgery. Regular monitoring helps adjust care plans effectively.
Overuse Injuries and Activity-Induced Pain
Daily routines often hide surprising risks for joint stress. Repetitive motions—like climbing stairs or cycling—create microscopic tears in tendons and cartilage. Over weeks, these tiny injuries accumulate, causing persistent discomfort during movement.
Body weight plays a critical role. Each extra pound adds four pounds of pressure to the joint during bending. High-impact activities like basketball or running amplify this strain, accelerating tissue wear.
Effective management starts with smarter movement patterns. Low-impact alternatives reduce stress while maintaining fitness:
| High-Impact | Low-Impact | Benefit |
|---|---|---|
| Running | Swimming | Reduces compression |
| Jumping | Cycling | Preserves cartilage |
| Tennis | Yoga | Improves flexibility |
Targeted exercises strengthen supporting muscles. Quadriceps and hamstring routines stabilize the joint, while balance drills improve alignment. As one study notes:
“Structured rehab programs decrease overuse injury recurrence by 38% compared to rest alone.”
For chronic cases, physical therapy offers customized solutions. Therapists assess gait abnormalities and recommend orthotics or activity modifications. Early intervention helps manage symptoms before they limit mobility.
Adjusting workout frequency and intensity prevents flare-ups. Alternating high-stress days with recovery periods allows tissues to heal. Listen to your body—persistent soreness signals the need for professional evaluation.
Home Remedies and Self-Care Strategies
Managing discomfort during daily movements starts with smart self-care techniques. Simple adjustments often reduce strain and promote healing, even without medical intervention. Let’s explore proven methods to support your body’s recovery process.
Implementing the PRICE Method
The PRICE protocol addresses acute irritation effectively. This five-step approach minimizes tissue stress:
| Step | Action | Benefit |
|---|---|---|
| Protection | Avoid aggravating movements | Prevents further damage |
| Rest | Limit activity for 24–48 hours | Allows tissue repair |
| Ice | Apply cold packs for 15-minute intervals | Reduces swelling |
| Compression | Use elastic bandages | Supports joint stability |
| Elevation | Keep leg raised above heart level | Improves fluid drainage |
This method works particularly well for front knee discomfort caused by overexertion. Ice application remains crucial—research shows cold therapy lowers internal swelling by 30% within 72 hours.
Effective Stretching and Low-Impact Exercises
Gentle movement maintains flexibility while preventing stiffness. Focus on these activities:
| Exercise | Frequency | Target Area |
|---|---|---|
| Hamstring stretches | 3x daily | Back of thigh |
| Straight-leg raises | 2 sets of 10 | Quadriceps |
| Water aerobics | 3x weekly | Full-body support |
Low-impact options like swimming or cycling help prevent cartilage wear. Pair these with posture adjustments during sitting or standing to distribute weight evenly. Remember: home care complements professional treatment but doesn’t replace evaluation for persistent issues.
Medical Diagnosis and Treatment Options
Accurate diagnosis forms the foundation of effective care for joint issues. Doctors combine physical assessments with advanced imaging to pinpoint underlying problems. This dual approach helps tailor solutions to each patient’s unique needs.
Imaging Tests and Physical Examinations
Your doctor will first assess movement patterns and tenderness locations. Range-of-motion tests reveal stiffness or instability. Palpation identifies swollen areas or abnormal tissue textures—even without visible inflammation.
Common imaging tools include:
| Test | Purpose | Best For |
|---|---|---|
| X-ray | Bone alignment check | Fractures, arthritis |
| MRI | Soft tissue analysis | Ligament tears, cartilage damage |
“MRI scans detect 92% of meniscus injuries missed by physical exams alone,” notes a Johns Hopkins orthopedic study.
Non-Surgical Versus Surgical Interventions
Most conditions respond well to conservative methods. Physical therapy strengthens supporting muscles, while anti-inflammatory medications reduce discomfort. Custom orthotics often correct alignment issues contributing to strain.
When non-invasive approaches fail, surgical options emerge:
| Approach | Benefits | Considerations |
|---|---|---|
| Arthroscopy | Minimal scarring | 3–6 week recovery |
| Joint Replacement | Long-term relief | 6-month rehab |
Treatment plans evolve based on progress tracking. Regular follow-ups ensure strategies remain aligned with healing milestones. Always discuss potential risks and success rates with your healthcare provider.
The Role of Physical Therapy and Rehabilitation
Restoring mobility after joint stress requires more than rest—it demands strategic movement. Modern rehabilitation focuses on rebuilding strength while protecting vulnerable tissues. Targeted plans address both immediate discomfort and long-term resilience.
Strengthening and Flexibility Exercises
Customized routines reactivate weakened muscles without overloading joints. Quadriceps activation drills, like mini squats, improve stability during daily movements. A recent study emphasizes:
“Patients completing structured rehab programs regain 89% of pre-injury flexibility compared to 62% with rest alone.”
Effective regimens often include these components:
| Exercise Type | Muscle Group | Frequency |
|---|---|---|
| Step-ups | Quadriceps | 3x weekly |
| Hamstring curls | Back of leg | Daily |
| Calf raises | Lower leg | Every other day |
Balance training proves equally vital. Single-leg stands challenge proprioception, reducing reinjury risks. Therapists frequently combine these with soft tissue mobilization to enhance range of motion.
Collaboration between patients and specialists ensures optimal progress. Adjustments to exercise intensity prevent setbacks while promoting gradual improvement. This partnership transforms recovery from passive waiting to active empowerment.
Preventative Measures and Lifestyle Adjustments
Protecting joint health requires daily attention to habits that support mobility. Small, consistent changes often yield the most significant long-term benefits. Let’s explore actionable strategies to maintain flexibility and reduce strain.
Weight Management and Activity Modification
Excess body mass multiplies pressure on joints during movement. Research shows losing 10 pounds reduces force on lower limbs by 40 pounds per mile walked. Focus on nutrient-rich diets paired with sustainable exercise routines to achieve gradual weight loss.
Adjusting physical activities prevents repetitive stress injuries. Swap high-impact workouts for gentler alternatives:
| High-Impact | Low-Impact | Benefit |
|---|---|---|
| Running | Elliptical training | Reduces shock absorption |
| Basketball | Tai Chi | Improves balance |
“Patients who modified exercise intensity reduced overuse injuries by 67% compared to those maintaining previous routines,” states a 2023 sports medicine review.
People prone to band syndrome should avoid prolonged kneeling or squatting. Incorporate rest days between intense workouts to allow tissue recovery. Simple daily adjustments—like using ergonomic chairs or supportive footwear—help maintain proper alignment.
Building muscle strength around joints through resistance training enhances stability. Combine this with stretching to improve flexibility. These proactive steps create a foundation for lasting mobility, letting you stay active without compromising comfort.
Conclusion
Recognizing the root of movement-related discomfort transforms uncertainty into actionable solutions. Our exploration reveals how front-line injuries, degenerative conditions, and mechanical stress interact within complex biological systems.
Accurate diagnosis combines imaging technology with hands-on assessments. Treatment plans thrive when merging self-care strategies with professional guidance. Strengthening exercises, activity modifications, and timely medical consultations form a three-pillar defense against chronic issues.
Persistent symptoms demand attention—consulting a doctor prevents minor irritations from escalating. Advanced imaging and physical therapy often restore function without invasive measures. Remember: your joint health reflects daily choices as much as genetic factors.
Stay vigilant through these steps:
- Track symptom patterns during daily activities
- Prioritize low-impact exercises that protect tissues
- Schedule evaluations at the first sign of recurring discomfort
Proactive care preserves mobility better than reactive treatments. By understanding your body’s warning signals, you maintain control over long-term wellness.
