
If you’re dealing with persistent knee pain below the kneecap, you’ve likely heard conflicting advice. Should you push through discomfort to build flexibility, or could certain movements damage sensitive tissues? For active individuals managing Osgood-Schlatter Disease, this question defines their rehabilitation journey.
We’ve worked with dozens of athletes navigating this condition. While gentle movement supports recovery, aggressive approaches often backfire. The inflamed tibial tuberosity – that bony bump beneath the knee – requires precise care. Timing matters more than intensity when working with developing growth plates.
Many assume stretching automatically reduces discomfort. But during acute flare-ups, even basic quadriceps stretches can strain irritated tendons. Our approach prioritizes low-impact techniques that balance mobility with protection. You’ll learn which methods to use (and avoid) based on your pain levels and activity goals.
Key Takeaways
- Stretching benefits depend entirely on proper form and timing
- Avoid aggressive techniques during active inflammation phases
- Focus on stabilizing muscles around the knee joint
- Growth plate sensitivity varies by age and activity level
- Combine stretching with strength exercises for lasting results
Introduction to Osgood-Schlatter Disease and Its Impact
A tender lump below the kneecap often marks the start of a frustrating journey for active adolescents. Unlike typical muscle soreness, this condition stems from repeated stress on developing bones during growth spurts.
Overview of Symptoms and Causes
Young athletes frequently report three telltale signs: localized swelling, tenderness when kneeling, and sharp knee pain during explosive movements like jumping. The discomfort centers around the tibial tuberosity – the bony attachment point for the patellar tendon. Growth plates here remain vulnerable until skeletal maturity, making them prone to inflammation from repetitive strain.
Common triggers include:
- Sports requiring frequent direction changes (basketball, soccer)
- Sudden increases in training intensity
- Poor landing mechanics during jumps
Why Recovery and Mobility Matter
Ignoring early symptoms risks long-term complications. Recovery-focused exercises maintain joint function without aggravating inflamed tissues. A physical therapist we collaborate with notes: “Controlled movement preserves range of motion while allowing natural healing – it’s about working smarter, not harder.”
Strategic approaches prioritize:
- Low-impact activities that reduce tendon tension
- Strengthening supporting muscles (hamstrings, glutes)
- Modifying training volumes during growth spurts
Early intervention helps athletes stay active while protecting developing bones. Always consult a sports medicine specialist when pain interferes with daily activities.
Understanding Osgood-Schlatter Disease
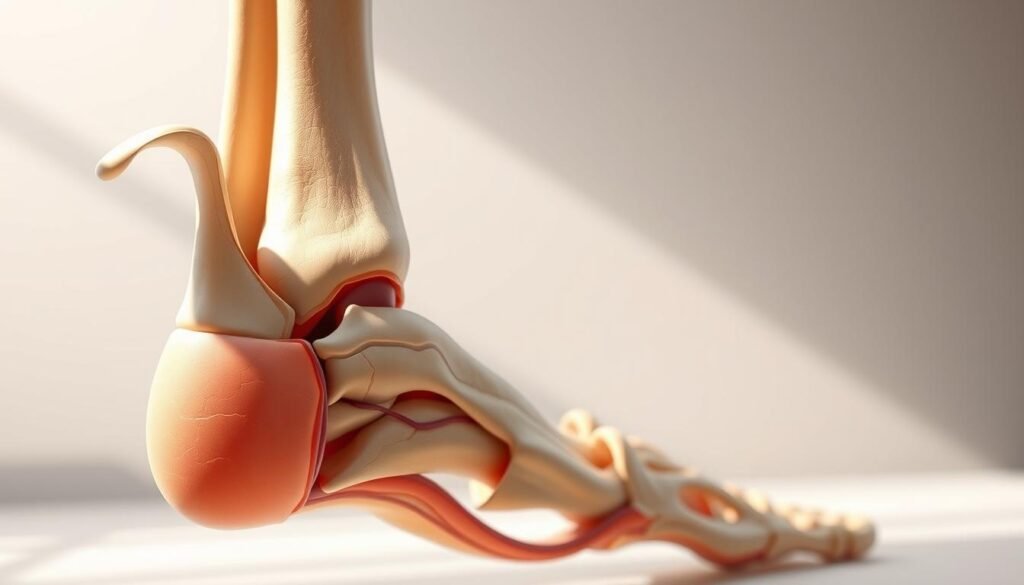
The knee’s complex structure becomes particularly vulnerable during growth spurts. At the center of this condition lies the tibial tuberosity – a raised area on the shinbone where the patellar tendon anchors. This connection point undergoes significant stress during activities that involve jumping or rapid direction changes.
Exploring the Tibial Tuberosity and Growth Plate
During adolescence, the growth plate near the tibial tuberosity remains soft and cartilage-like. Repeated tension from the patellar tendon can create micro-tears, leading to inflammation and that characteristic bump below the knee. Sports medicine specialists emphasize this area’s sensitivity: “The developing bone can’t keep pace with muscle growth during rapid height changes,” explains Dr. Ellen Torres, orthopedic surgeon.
| Age Group | Growth Plate Status | Injury Risk |
|---|---|---|
| 10-13 years | Most active growth | Highest vulnerability |
| 14-16 years | Partial closure | Moderate risk |
| 17+ years | Fully closed | Low risk |
Who Is Affected and Why?
Active teens involved in sports like basketball or soccer face the highest likelihood of developing osgood-schlatter disease. Studies show 21% of adolescent athletes experience symptoms compared to 4.5% of non-athletes. Contributing factors include:
- Frequent explosive leg movements
- Tight quadriceps muscles
- Improper footwear
While exercises osgood-schlatter patients perform can aid recovery, starting any regimen without medical advice risks worsening inflammation. Physical therapists often recommend activity modifications alongside targeted mobility work to protect the developing joint structures.
Role of Stretching in Osgood Recovery
Many assume stretching is universally beneficial for knee issues, but timing and technique dictate outcomes. When inflammation flares, aggressive approaches can worsen discomfort. Strategic stretching targets muscle groups influencing the patellar tendon without stressing vulnerable growth areas.
How Gentle Stretching Aids Healing
Tight quadriceps and hamstrings pull excessively on the patellar tendon, intensifying knee pain. A physical therapist we collaborate with explains: “Gentle lengthening of these muscles reduces tension on the tibial tuberosity, creating space for natural healing.” This approach works best when combined with rest periods to avoid overloading tissues.
Effective programs prioritize three elements:
- Holding stretches for 20-30 seconds (no bouncing)
- Focusing on breath control to prevent strain
- Stopping immediately if sharp pain occurs
Research shows gradual recovery plans incorporating low-intensity exercise improve mobility 37% faster than complete rest. However, pushing through discomfort during growth spurts risks permanent bumps below the kneecap. Athletes should modify their program weekly based on pain levels and swelling.
Consistency matters more than intensity. Daily 10-minute sessions maintain muscle elasticity better than hour-long weekly routines. Pair stretching with strength-building exercises for balanced recovery – we’ll explore specific techniques in later sections.
Our Best Stretches for Osgood Schlatters
Strategic movement patterns can ease tension around sensitive knee areas while supporting long-term joint health. Our clinical team developed these four evidence-based techniques through work with adolescent athletes managing growth-related discomfort.
Crouching Adductor and Kneeling Hip Flexor Stretches
Tight inner thigh muscles often contribute to knee misalignment. The crouching adductor stretch:
- Stand with feet wider than shoulder-width
- Lower into partial squat, keeping heels grounded
- Place elbows inside thighs for gentle outward pressure
For hip flexors, use a cushioned surface. “Kneeling stretches require padding to protect the tibial tuberosity,” advises physical therapist Marco Rodriguez. Hold each position 20 seconds, breathing deeply to enhance body relaxation.
Lying Glute and Standing Calf Techniques
Imbalanced quadriceps strength frequently accompanies this condition. The lying glute stretch:
- Lie on back with knees bent
- Cross right ankle over left thigh
- Gently pull left leg toward chest
Pair this with standing calf stretches against a wall. These methods improve strength distribution across the lower body, reducing strain on vulnerable areas. Always modify based on daily symptoms – some days may require shorter holds or extra padding.
Consistent practice helps maintain mobility during growth phases. Combine these movements with professional guidance to address individual recovery needs effectively.
Foam Rolling: An Essential Pre-Stretch Technique
Many athletes overlook a crucial step before stretching – preparing muscles through targeted pressure. Foam rolling offers a safer alternative to direct stretching during active growth phases, particularly for those managing osgood-schlatter disease. Unlike traditional methods, this approach reduces tension in surrounding tendon networks without stressing vulnerable areas.
Benefits Over Direct Muscle Stretching
Foam rolling works through myofascial release, gradually improving mobility by breaking up muscle adhesions. A sports therapist from our network explains: “This technique warms tissue layers sequentially, making subsequent stretches more effective and less jarring for inflamed areas.”
Key advantages include:
- Reduced risk of overstretching irritated tendon attachments
- Improved blood flow to quadriceps and hamstrings
- Customizable pressure based on daily symptoms
| Technique | Pressure Applied | Target Area | Risk Level |
|---|---|---|---|
| Foam Rolling | Gradual, controlled | Muscle bellies | Low |
| Static Stretching | Sustained tension | Tendon junctions | Moderate |
Protecting the Sensitive Knee Area
Proper form prevents aggravating the tibial tuberosity. Keep the roller mid-thigh, avoiding direct contact with the bony bump below the knee. Our treatment protocols recommend 2-3 minute sessions focusing on:
- Outer thigh (IT band)
- Front thigh (quadriceps)
- Back thigh (hamstrings)
Research shows combining foam rolling with sports massage and stretching techniques improves mobility 28% faster than stretching alone. This method proves especially valuable during growth spurts when tissues need gentle treatment approaches.
Consistent use helps maintain muscle elasticity, a critical part of long-term osgood-schlatter disease management. Always pair rolling with medical guidance to address individual recovery needs effectively.
Safe Stretching Techniques to Avoid Injury
What separates helpful stretching from harmful strain? Proper technique determines whether movements support healing or prolong discomfort. Our clinical team observes that rushed routines often undo weeks of progress, especially when dealing with sensitive growth areas.

Guidelines on Timing and Intensity
Aggressive stretching ranks among the top mistakes we correct. Bouncing or forcing the leg into extreme positions strains the patellar tendon, worsening inflammation. Instead, hold stretches at 70% capacity – if you feel tension but no sharp pain.
Timing matters for two reasons:
- Morning sessions often feel tighter due to overnight stiffness
- Post-activity stretching works best when muscles are warm
Avoid direct pressure on the tuberosity during routines. For running or jumping drills, focus on soft landings with bent knees. As one athlete shared: “Learning to absorb impact through my hips instead of knees changed everything.”
Modify holds based on daily symptoms. Reduce duration by 50% during flare-ups, using yoga blocks or straps to limit range. This way maintains mobility without overloading healing tissues.
Proper form during dynamic activities protects the patellar tendon. Keep feet aligned under hips when changing directions, and avoid locking knees at the top of jumping motions. These adjustments distribute forces safely – a smarter way to stay active while respecting the tuberosity‘s healing timeline.
Integrating Strength Training with Stretching
Building strength while maintaining flexibility creates a protective framework for developing joints. Our work with adolescent athletes shows that combining these approaches reduces strain on the site of injury while improving overall movement patterns. A physical therapist from our network states: “Targeted resistance work helps muscles absorb forces that would otherwise stress the growth plate.”
Incorporating Isometric Exercises and Modified Squats
Isometric holds like wall sits teach muscles to stabilize without joint movement. Try this approach:
- Lean against wall with knees bent at 45 degrees
- Hold position 15-20 seconds
- Focus on even weight distribution
Modified squats using limited range of motion protect the tibial tuberosity. Keep heels elevated on a low platform to reduce tendon tension. These methods strengthen quadriceps and glutes without overloading the site of inflammation.
Glute Bridges and Core Stability Work
Weak core muscles force the knees to compensate during activities. Glute bridges activate posterior chains safely:
- Lie on back with knees bent
- Lift hips until body forms straight line
- Squeeze glutes at top position
Adding planks or bird-dog exercises improves trunk stability. This redistribution of forces helps shield the growth plate during growth spurts. For those managing osgood schlatter, alternating strength days with stretching sessions yields better long-term results than either approach alone.
Movement and Mobility: Beyond Simple Stretching
Movement efficiency often determines how forces travel through developing joints. While stretching addresses muscle tightness, refining movement patterns redistributes stress away from vulnerable areas. This approach helps athletes maintain activity levels while protecting healing tissues.
Improving Jumping, Landing, and Running Mechanics
Proper timing during high-impact activities reduces strain on the growth area. A track coach we collaborate with notes: “Teaching athletes to land softly through their midfoot – not heels – cuts impact forces by 40%.”
Key adjustments include:
- Bending knees to 30° upon landing
- Keeping hips aligned over knees during direction changes
- Shortening stride length when running
These positional changes shift tension from the knee to stronger muscle groups. For example, wall drills that emphasize hip extension improve force distribution across the entire leg area.
Growth phases require ongoing modifications. Use video analysis every 4-6 weeks to track progress. Pair this with single-leg balance exercises to enhance dynamic stability. Athletes who follow this guide typically see fewer symptom flare-ups during competitive seasons.
Remember: Movement retraining takes time. Start with 5-minute skill sessions post-warmup, gradually increasing complexity. Proper mechanics become automatic when practiced consistently – a critical step for long-term joint health.
Common Mistakes and Troubleshooting Your Routine
Your body sends clear signals during recovery – learning to interpret them prevents setbacks. Many athletes mistake discomfort for progress, pushing through pain that indicates tissue irritation. This misunderstanding often stems from outdated information about “no pain, no gain” mentalities.
Identifying Signs of Overstretching and Sharp Pain
The mechanism behind overstretching involves excessive force on partially healed tendons. When the patellar tendon pulls too hard on the tibial tuberosity, it creates micro-tears that delay healing. A sports medicine specialist we consulted notes: “Sharp pain during stretching means you’re loading damaged tissue – it’s your body’s stop sign.”
Differentiate between productive tension and harmful strain:
| Safe Signal | Warning Sign | Action Required |
|---|---|---|
| Mild pulling sensation | Localized stabbing pain | Stop immediately |
| Gradual release | Increased tightness post-stretch | Reduce intensity |
| Symmetrical flexibility | One-sided discomfort | Consult professional |
Running enthusiasts often face unique challenges. Impact forces during gait cycles can reactivate inflammation if stretching routines lack proper modifications. Track these symptoms:
- Persistent warmth around the knee after activity
- Difficulty straightening the leg fully
- Visible swelling near the tibial tuberosity
Our advice: Keep a symptom journal to spot patterns. If morning tightness lasts over 30 minutes, reduce stretching duration by 25%. Pair this information with activity modifications – swap pavement running for pool workouts during flare-ups.
Remember, the healing mechanism works best when supported by smart adjustments. Use this article‘s checklist to refine your routine weekly, prioritizing tissue response over rigid schedules.
Recovery Programs and Professional Guidance
Managing growth-related knee conditions requires more than cookie-cutter solutions. Our work with youth sports teams reveals a critical truth: osgood-schlatter disease responds best to personalized plans that evolve with physical changes. One physical therapist puts it bluntly: “Trying to force standard protocols often worsens irritation – flexibility in programming is non-negotiable.”
When to Consult Medical Professionals
Persistent symptoms demand expert evaluation. Seek immediate guidance if you notice:
| Symptom | Duration | Action |
|---|---|---|
| Swelling near tuberosity | 3+ days | Schedule imaging |
| Limited leg motion | 2 weeks | Physical therapy consult |
| Pain during walking | 1 week | Activity modification |
Sports medicine specialists assess tendon tension patterns and growth plate status through hands-on tests. They might recommend:
- Gait analysis to identify movement imbalances
- Cross-training plans preserving mobility
- Bracing options during acute phases
Customizing Your Exercise Program
Effective routines adapt to daily fluctuations in tuberosity sensitivity. Track these three factors weekly:
| Metric | Green Zone | Adjustment Needed |
|---|---|---|
| Morning stiffness | <15 minutes | Reduce stretching intensity |
| Post-activity irritation | 0-2/10 pain | Modify impact exercises |
| Leg mobility range | 90% of healthy side | Increase foam rolling |
Young athletes often benefit from alternating strength days with active recovery sessions. A collegiate soccer coach shares: “We pair isometric holds with pool workouts during growth spurts – keeps players moving without overloading tender areas.” This approach maintains conditioning while respecting the body’s healing timeline.
Remember: Progress isn’t linear. Regular professional check-ins ensure your program addresses changing needs as bones mature and activity levels shift.
Conclusion
Navigating knee discomfort during growth phases requires a balanced approach. Our guidance emphasizes three pillars: strategic stretching, targeted strength work, and movement pattern refinement. These elements work together to reduce tendon tension while supporting developing joints.
Successful recovery hinges on adapting your program to daily symptoms. Track changes in stiffness or swelling, adjusting exercise intensity accordingly. “Progress often comes through subtle tweaks, not drastic changes,” notes a sports therapist we collaborate with.
Key takeaways include:
- Pair low-impact mobility drills with isometric holds
- Prioritize muscle balance over aggressive stretching
- Consult professionals when pain limits daily activities
View this article as your roadmap for managing symptoms while staying active. Implement one technique at a time, allowing your body to adapt. With consistent effort and expert guidance, athletes can maintain performance while protecting vulnerable growth areas.
