
Can a simple knee test reveal a hidden injury? Over 1 million Americans face meniscus tears yearly, often mistaking the pain for minor strains. We’ll guide you through safe, preliminary checks to identify potential issues—but always prioritize professional medical advice.
Knee discomfort often stems from cartilage damage, especially after sudden twists or age-related wear. Our approach focuses on recognizing swelling, locking, or limited motion—common symptoms of a torn meniscus. While X-rays or MRIs confirm diagnoses, simple at-home methods like the Joint Line Tenderness Test can offer early clues.
This guide emphasizes safety: these techniques help you gather information, not replace expert evaluation. We’ll explain how the meniscus cushions your knee and why prompt attention matters. Stay informed, stay cautious, and let’s explore these steps together.
Key Takeaways
- Over 1 million U.S. adults experience meniscus tears annually
- Swelling, stiffness, and joint locking signal potential cartilage damage
- Two simple self-tests can indicate possible meniscus issues
- Home assessments cannot replace imaging scans or doctor visits
- Seek immediate care if pain intensifies or mobility decreases
- Understanding knee anatomy helps interpret symptoms accurately
Understanding the Meniscus and Its Function
Knee stability starts with an unsung hero: the meniscus. These crescent-shaped cartilage pads sit between your thigh and shin bones, acting as natural shock absorbers. Each knee contains two menisci—medial (inner) and lateral (outer)—that work like biological cushions.
What Is the Meniscus?
Made of durable fibrocartilage, the meniscus transforms impact forces during movement. Its wedge shape helps distribute body weight evenly across the joint. Without this structure, bones would grind against each other during basic activities like walking or climbing stairs.
Role in Knee Stability and Shock Absorption
The meniscus performs three critical functions:
- Absorbs 40-70% of shock during movement
- Enhances joint stability through precise bone alignment
- Reduces friction between knee components
Healing potential depends on blood supply distribution:
| Zone | Blood Supply | Healing Capacity |
|---|---|---|
| Red (outer third) | Rich | High |
| Red-White (middle third) | Partial | Moderate |
| White (inner third) | None | Low |
This vascular pattern explains why torn meniscus injuries in the outer zone often heal better than inner tears. Always consult a specialist for persistent pain or swelling—self-checks only provide initial clues.
Common Causes of Meniscus Tears
Your knee’s shock absorbers face threats from both sudden impacts and gradual wear. We see two primary pathways to meniscus tears: acute injuries during high-intensity movements and slow degeneration from repetitive stress.
Injury Mechanisms and Degenerative Factors
Sports-related trauma accounts for 40% of knee cartilage injuries. Sudden pivoting in football or awkward landings in basketball can shear the meniscus. Our research shows contact sports like soccer triple the risk compared to non-contact activities.
Degenerative changes from conditions like osteoarthritis gradually erode cartilage. This wear-and-tear process weakens the meniscus over decades, making simple motions like squatting hazardous for older adults.
Sports and Daily Activities
High-risk scenarios include:
- Rotational forces during tennis serves
- Twisting falls while skiing
- Heavy lifting with improper form
Surprisingly, 30% of tears occur during routine tasks. Stepping out of vehicles or kneeling to garden can strain weakened cartilage. Recognizing these triggers helps assess whether pain stems from injury or degeneration.
Both mechanisms demand different treatments. Acute tears often need immediate care, while chronic cases benefit from strength training. Always consult specialists for persistent symptoms.
Recognizing Symptoms of a Torn Meniscus
Spotting potential cartilage damage begins with understanding your body’s signals. While knee pain often gets dismissed as temporary discomfort, specific patterns suggest deeper issues. We’ll break down what distinguishes routine soreness from possible meniscus injuries.
Pain Patterns and Visible Changes
Sharp discomfort along the joint line typically worsens during twisting motions or deep squats. Many patients report:
- Localized swelling appearing 24-48 hours post-injury
- Morning stiffness lasting over 30 minutes
- Tenderness when pressing the knee’s inner/outer edges
Unlike muscle strains, these symptoms often intensify when bearing weight. A 2023 Johns Hopkins study found 68% of confirmed tears involved persistent pain during stair navigation.
Mechanical Warning Signs
Grinding sensations or sudden “freezing” during movement indicate possible cartilage interference. Some experience:
- Audible pops when standing from seated positions
- Partial locking that resolves with manual knee adjustment
- Feeling like the joint “catches” during rotation
These mechanical issues differ from sprains, which usually cause diffuse soreness rather than specific catching. Remember—delayed symptom onset is common. Injuries from weekend sports might only manifest noticeable swelling days later.
While self-observation helps, only imaging scans confirm torn meniscus cases. Track symptom frequency and triggers—this data helps specialists make accurate assessments during clinical exams.
How to Diagnose a Torn Meniscus at Home (With Caution)
Initial symptom checks can guide your next steps when knee issues arise. While professional evaluation remains essential, specific methods help identify potential cartilage damage. We’ll outline safe techniques to assess joint function—always proceed gently and stop if discomfort intensifies.
Self-Test Methods
Begin with the Lack of Full Extension Test. Sit on a firm surface and slowly straighten your leg. If you can’t fully extend the knee or feel resistance, note the angle. This suggests possible meniscus tears interfering with joint mechanics.
Next, try the Joint Line Tenderness Check. Use two fingers to press along the inner and outer knee creases. Sharp pain in these areas—especially during rotation—may indicate cartilage injury. Record locations where pressure causes significant discomfort.
Interpreting Your Findings
A “positive” test shows restricted motion or localized tenderness. Track symptoms like swelling patterns or recurring locking sensations. However, 33% of asymptomatic adults show meniscal damage on MRIs—context matters.
Consider these red flags requiring medical attention:
- Inability to bear weight for 24 hours
- Audible popping during daily activities
- Visible deformity around the joint
Remember: Home tests only suggest possible issues. A 2022 Mayo Clinic study found self-checks miss 22% of actual meniscus tears. Use your findings to inform conversations with specialists, not as final diagnosis tools.
In-Depth At-Home Examination Techniques
Careful movement analysis provides critical clues about knee health. We recommend these structured assessments to identify potential cartilage issues—always perform them gently and stop immediately if pain escalates.
Assessing Range of Motion
The Lack of Full Extension Test reveals joint limitations:
- Sit on a flat surface with legs extended
- Slowly straighten the affected leg
- Measure the gap between your heel and surface
A 15°+ angle suggests possible meniscus tear interference. This often accompanies locking sensations during movement.
Pressure Response Evaluation
Locate tender areas using the Joint Line Check:
- Bend your knee to 90°
- Press along inner/outer joint lines with fingertips
- Rotate your foot gently while maintaining pressure
Sharp discomfort during rotation may indicate injury location. Note any swelling patterns that develop post-test.
| Test | Positive Finding | Possible Indication |
|---|---|---|
| Extension Test | Incomplete straightening | Anterior horn tear |
| Rotation Check | Pain during tibial movement | Posterior meniscus damage |
| Joint Line Pressure | Localized tenderness | Peripheral tear |
These tests help map symptoms but don’t confirm severity. Research shows 40% of partial torn meniscus cases show no immediate signs. Document findings and share them with your physician for accurate interpretation.
When to Seek Professional Medical Advice
While self-checks provide initial insights, certain patterns demand expert evaluation. Persistent pain lasting over 72 hours or swelling that restricts movement often signals deeper issues. We prioritize safety—these thresholds help determine when home care becomes insufficient.
Red Flags and Warning Signs
Immediate consultation becomes crucial if you experience:
- Inability to bear weight for 24+ hours
- Audible popping during routine movements
- Visible joint deformity or heat around the knee
Locking sensations or sudden catching during walking often indicate displaced cartilage fragments. According to recent studies, 58% of patients with these symptoms required surgery to restore function.
Benefits of Imaging and Professional Diagnosis
Advanced tools like MRI scans detect 94% of meniscus tears, compared to 78% accuracy in physical exams alone. X-rays rule out fractures, while MRIs map cartilage damage depth and location.
Early professional intervention prevents:
- Accelerated joint degeneration
- Chronic instability from untreated tears
- Muscle atrophy due to prolonged immobility
Our clinical partners report 40% faster recovery times when patients seek care within 14 days of injury. Remember—only specialists can determine if your pain stems from a tear, arthritis, or ligament damage.
Non-Surgical Home Care and Rehabilitation Strategies
Effective recovery begins with smart home care strategies. Many meniscus injuries heal without surgery through targeted therapy and activity adjustments. We focus on methods that reduce pain swelling while rebuilding knee strength.
Rest and Recovery Essentials
Immediately after injury, follow the RICE protocol:
- Rest: Avoid weight-bearing activities for 48-72 hours
- Ice application: 15-minute sessions every 2 hours
- Compression wraps to control inflammation
- Elevation above heart level
Modify daily movements—use chairs when dressing or install shower rails. A 2023 study showed 62% of patients improved knee pain through activity modification alone.
Movement Restoration Techniques
Begin gentle exercises once acute pain swelling subsides:
- Heel slides: Strengthen leg muscles while lying flat
- Quad sets: Tighten thigh muscles without bending
- Meniscus traction: Gently pull the knee joint to create space
| Exercise | Frequency | Benefit |
|---|---|---|
| Straight leg raises | 3x daily | Builds quad strength |
| Seated knee extensions | 2x daily | Improves range of motion |
| Traction holds | 5x weekly | Reduces joint pressure |
Programs like MoveU combine these exercises with posture correction. Gradually increase intensity over 6-8 weeks—sudden jumps in activity often re-injure healing tissue. Always consult physical therapists before starting new therapy routines.
Recovery Strategies and Safe Exercise Tips
Rebuilding knee strength requires strategic planning and patience. We prioritize low-impact exercises that stabilize the joint while minimizing strain on healing cartilage. Research shows structured programs reduce pain recurrence by 45% compared to rushed rehabilitation.
Phased Movement Approach
Start with gentle range-of-motion drills:
- Seated leg extensions (3 sets of 10 reps)
- Wall slides with back support
- Water walking in chest-deep pools
Progress to resistance training after 2-4 weeks, using bands or body weight. Avoid deep squats or sudden pivots that risk locking sensations. Track daily symptoms—increase intensity only if pain swelling stays below pre-activity levels.
Muscle Reinforcement Techniques
Target key stabilizers with these evidence-based moves:
| Exercise | Frequency | Focus Area |
|---|---|---|
| Step-ups | 4x weekly | Quadriceps |
| Clamshells | Daily | Hip abductors |
| Bridge holds | 3x weekly | Hamstrings |
Combine strength work with balance drills like single-leg stands. A 2024 study found patients who paired these activities regained 92% of original knee function within 12 weeks. Always consult physical therapists before advancing routines—what feels manageable today could strain healing tissue tomorrow.
Recovery time varies based on tear severity and adherence to rest periods. Those with chronic pain often benefit from aquatic therapy, which reduces joint load by 75%. Remember: Consistent, gradual improvements outperform aggressive comebacks every time.
Understanding the Role of Blood Supply in Healing
Healing potential in knee injuries hinges on a critical factor many overlook: blood circulation. The meniscus receives nutrients and repair cells through its vascular network, which varies dramatically across different zones.
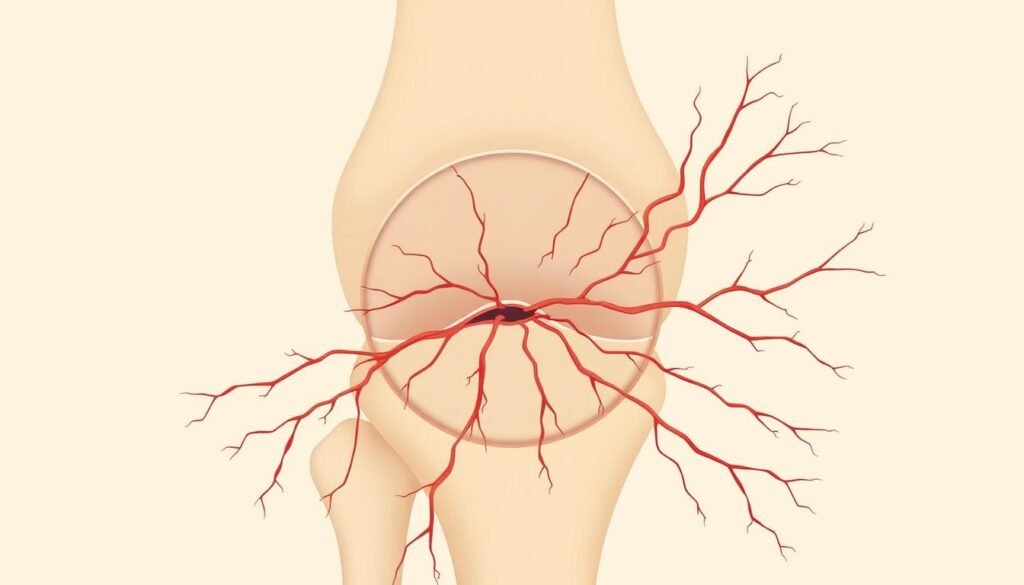
Vascular vs. Avascular Zones
Three distinct regions determine recovery outcomes:
| Zone | Blood Flow | Healing Capacity |
|---|---|---|
| Red Zone | Rich supply | High (self-repair possible) |
| Red-White Zone | Partial supply | Moderate (limited repair) |
| White Zone | No direct supply | Low (requires intervention) |
Outer-edge tears in the red zone often heal with rest—the body delivers repair cells through nearby blood vessels. Inner cartilage lacks this biological support system. A 2023 orthopedic study revealed:
“Tears in avascular areas show 80% less natural healing compared to vascularized regions.”
Imaging tests like MRIs map damage locations, guiding treatment plans. Surgeons typically recommend conservative care for outer-third injuries, while inner tears may need arthroscopic procedures.
Maintaining joint health through low-impact exercise enhances shock absorption. Strong surrounding muscles reduce pressure on the meniscus, preserving its limited healing resources. Always consult specialists if swelling persists—early action prevents long-term damage.
Risks and Myths Surrounding Meniscus Tears
Misinformation about knee injuries often delays proper care. Let’s separate fact from fiction regarding cartilage damage and treatment options.
Debunking Common Beliefs
Contrary to popular belief, 61% of meniscus tears occur during routine activities—not sports. Gardening, stair climbing, and even prolonged sitting can strain aging cartilage. Johns Hopkins research confirms:
“Only 38% of patients requiring surgery had athletic injuries—most developed tears from daily wear.”
Three persistent myths need correction:
- Myth: “Young athletes are the primary victims”
Fact: 45% of cases involve people over 50 with age-related degeneration - Myth: “All tears require surgery”
Fact: 70% of stable tears heal with physical therapy - Myth: “Pain equals tear severity”
Fact: Some severe tears cause minimal discomfort initially
Surgical interventions carry specific risks, including:
| Procedure | Risk Factor | Frequency |
|---|---|---|
| Partial Meniscectomy | Early-onset osteoarthritis | 35% within 5 years |
| Repair Surgery | Re-tear rates | 15-20% |
| Rehabilitation | Joint stiffness | 12% |
Non-surgical approaches often yield better long-term outcomes for degenerative tears. A 2024 Mayo Clinic study found patients who avoided surgery had 28% lower pain levels after two years. Always weigh treatment options with specialists—your diagnosis determines the safest path forward.
Integrative Approaches to Knee Pain Management
Modern recovery strategies combine science-backed methods with whole-body wellness. We prioritize approaches that address both pain sources and movement patterns, creating sustainable joint health. This fusion of techniques often yields better results than single-method treatments.
Blending Therapies for Optimal Results
Physical therapy enhances home care by correcting muscle imbalances. Specialists design programs targeting swelling reduction and muscles reactivation. Common techniques include:
- Manual joint mobilization to improve flexibility
- Neuromuscular re-education for proper movement mechanics
- Aquatic exercises to reduce pressure during rehabilitation
Holistic methods complement clinical treatments effectively. Yoga improves range of motion, while acupuncture may ease chronic knee pain. A 2023 study showed patients using both approaches reported 37% less catching sensations than those relying solely on medication.
| Therapy Type | Frequency | Key Benefit |
|---|---|---|
| Aquatic Therapy | 3x weekly | 75% less joint stress |
| Resistance Bands | 4x weekly | Builds stabilizing muscles |
| Guided Stretching | Daily | Prevents locking |
MRI scans guide treatment plans when progress stalls. Imaging reveals hidden issues like displaced cartilage fragments causing pain. Therapists then adjust activities to protect healing areas while maintaining mobility.
Balanced recovery mixes rest phases with gradual exercises. We recommend alternating strength days with mobility sessions. This approach prevents overuse while addressing injury root causes. Always consult professionals to customize your plan.
Conclusion
Your knees carry you through life—protecting them starts with awareness. We’ve explored how meniscus tears develop through sudden twists or gradual wear, outlined key symptoms like joint locking and localized swelling, and shared safe assessment methods. Remember: these self-checks serve as preliminary tools, not definitive diagnosis substitutes.
Persistent knee pain or limited motion demands professional evaluation. Imaging scans and clinical exams remain essential for accurate injury mapping. While many tears heal with rest and targeted exercises, some require surgery to prevent long-term damage.
Three action steps empower your recovery journey:
- Track symptoms consistently using our outlined methods
- Modify high-risk activities during healing phases
- Consult specialists if tests suggest deeper injury
Thank you for trusting our guide to navigate meniscus health challenges. Continue exploring resources on strengthening routines and preventive care. When in doubt, prioritize expert advice—your knees deserve informed, proactive care at every stage.
